The story of Lisa, a spirited nine-year-old girl, is a testament to resilience, love, and the transformative power of neurofeedback therapy for trauma in healing developmental wounds.
A Storm Behind Bright Eyes
Lisa was adopted at four months old by Sarah and Mark, who were immediately captivated by her bright eyes and the possibilities they saw in her future. As she grew, Lisa became a whirlwind of emotions—a child who could be tender and loving one moment, then overwhelmed with anger the next. Her outbursts included yelling, defiance, hurtful name-calling, and at times, even physical aggression towards Sarah. These episodes left Sarah feeling trapped in what she described as “an abusive relationship I can’t leave,” while Mark grew increasingly concerned about the escalating disrespect and aggression.
At school, Lisa struggled with learning and maintaining friendships. She had been diagnosed with ADHD and learning differences, but traditional interventions weren’t making the expected impact. Teachers observed her refusing to follow instructions, arguing with authority figures, and deliberately provoking others. Beneath the turbulence, however, was a sweet girl longing for connection, especially with her mom.
The Invisible Wounds of Developmental Trauma
Unbeknownst to many, Lisa’s challenges were more than just behavioral quirks; they were echoes of developmental trauma that began even before she entered Sarah and Mark’s lives. Developmental trauma refers to exposure to adverse experiences during critical periods of brain development—in Lisa’s case, possibly in utero. Research indicates that stress hormones like cortisol can cross the placenta, affecting fetal brain development. If her birth mother experienced high levels of stress or trauma during pregnancy, Lisa’s nervous system might have been wired from the start to be on high alert, primed for survival rather than relaxation and learning.
This early wiring could explain why Lisa’s system was perpetually on edge. She lived in a constant state of hyperarousal, making it difficult for her to regulate her emotions and behavior. The world felt unpredictable and unsafe, leading her to react with defiance and aggression as protective mechanisms.
The Diagnostic Maze: Unraveling Trauma, ADHD, and ODD
When Lisa’s parents came to us for help, we faced the complex task of untangling her symptoms. She exhibited signs commonly associated with ADHD—difficulty focusing, impulsivity, and hyperactivity—as well as anxiety symptoms like restlessness and constant worry. Adding to the complexity were her oppositional behaviors and occasional physical aggression, often linked to Oppositional Defiant Disorder (ODD).
However, developmental trauma can manifest in ways that mimic these disorders, making differential diagnosis challenging. Misdiagnosing trauma as solely ADHD or ODD could lead to treatments that don’t address the root cause, potentially exacerbating her distress. It’s crucial to understand that Lisa’s behaviors were not simply defiance or inattention but responses to an overactivated stress response system.
A System on Edge: Beginning Neurofeedback Therapy
Our initial plan was to conduct a Quantitative Electroencephalogram (QEEG) to map Lisa’s brain activity and gain insights into her neurological patterns. However, Lisa was so on edge that she couldn’t sit still long enough for the assessment. Recognizing this hurdle, we decided to begin with Sensorimotor Rhythm (SMR) neurofeedback therapy for trauma, focusing on calming her hyperarousal.
Over six sessions, Lisa engaged in neurofeedback exercises designed to help her quiet her body and mind. Gradually, she began to exhibit better control over her movements and emotions, and her ability to focus improved. With her nervous system more regulated, we were able to proceed with the full QEEG assessment.
Unveiling the Brain’s Story
The QEEG revealed patterns consistent with trauma and anxiety-related dysregulation. Elevated high beta activity was associated with anxiety and hyperarousal, while reduced alpha activity indicated difficulty relaxing. Dysregulation in her frontal lobes pointed to challenges with executive functions like attention and impulse control. Connectivity issues between her limbic system and prefrontal cortex affected her ability to regulate emotions and impulses.
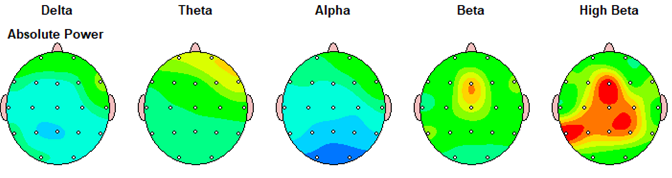
These findings suggested that while Lisa displayed behaviors similar to ADHD and ODD, the underlying issue was her brain being stuck in a state of constant alert due to trauma. Understanding this allowed us to tailor her treatment plan to address the root cause rather than just the symptoms.
Healing Through Neurofeedback Therapy for Trauma
We continued with neurofeedback sessions, now informed by the QEEG insights. The focus was on calming her hyperarousal by downtraining high beta activity and enhancing alpha activity to promote relaxation. We also worked on improving her frontal lobe functioning to aid in emotional regulation and executive functions. Strengthening the neural pathways between her limbic system and prefrontal cortex helped improve impulse control and reduce oppositional and aggressive behaviors.
Throughout this process, Lisa began to find moments of peace. She could sit through sessions more comfortably and started using coping strategies she learned, like deep breathing, to manage her emotions. The neurofeedback therapy was helping her brain develop healthier patterns, allowing her to move out of a perpetual fight-or-flight state.
The Power of Trauma-Informed Care Strategies
Parallel to the neurofeedback, Lisa participated in trauma-focused therapy. Here, she found a safe space to process her feelings and experiences. Art and play therapy techniques allowed her to express emotions that she couldn’t put into words. She began to understand her feelings better and learned that it was okay to have big emotions—but also how to handle them without lashing out.
Sarah and Mark were integral to Lisa’s healing journey. Through parent coaching, they learned trauma-informed care strategies to support their daughter:
- Building Safety and Predictability: Establishing consistent routines provided Lisa with a sense of security.
- Empathy and Validation: Acknowledging Lisa’s feelings helped reduce her defensiveness and build trust.
- Nonviolent Communication: Modeling calm and respectful interactions, even during conflicts, taught Lisa healthier ways to express herself.
- De-escalation Techniques: Recognizing early signs of agitation allowed them to intervene before aggression escalated.
By responding with empathy and validation, they helped Lisa feel understood and secure. They shifted from seeing her behaviors as willful defiance to viewing them as expressions of unmet needs—a key component of trauma-informed care.
Transformation and Hope
Over time, the changes in Lisa were profound. Incidents of physical aggression towards her mother decreased significantly. She learned to express her frustration through words or creative outlets rather than aggression. Her ability to self-regulate improved markedly; she could manage her emotions and behaviors more effectively.
At school, teachers noticed a positive shift. Lisa was more engaged in class, her focus improved, and she began to form healthier friendships. The academic improvements suggested that as her anxiety decreased, so did her attentional issues.
Most importantly, the family’s relationships strengthened. Lisa’s bond with her parents deepened as they all learned to communicate and connect in healthier ways. Even her interactions with her younger brother became more positive, with fewer conflicts and more cooperative play.
Expanding the Window of Tolerance
By addressing the primary issue—trauma—we expanded Lisa’s capacity to handle stress without becoming overwhelmed. This concept, known as the “window of tolerance,” refers to the zone in which a person can function effectively, even when faced with stressors. Neurofeedback therapy for trauma played a crucial role in calming her nervous system, enabling her to stay within this window more consistently.
Reflections on the Journey
Lisa’s story underscores the importance of meeting a child where they are. Recognizing that her system was too on edge for a full assessment, we adapted our approach, starting with interventions that helped her calm down before moving forward. This flexibility was key to engaging Lisa in her own healing process.
Her journey also highlights the necessity of comprehensive, trauma-informed care. By combining neurofeedback, counseling, and parent coaching, we addressed the multifaceted nature of her challenges. Understanding the overlap of symptoms in trauma, ADHD, anxiety, and ODD allowed us to avoid misdiagnosis and ineffective treatments.
A Message of Hope
Lisa’s transformation is a powerful reminder that healing is possible, even when the path is complex. With the right support and tools, children can overcome the shadows of early trauma. Neurofeedback therapy for trauma, guided by insights from QEEG and adapted to the child’s immediate needs, can be a potent component in a trauma-informed treatment plan.
If your child is exhibiting behaviors that are challenging to understand or manage, consider seeking a comprehensive evaluation that takes into account the potential impact of trauma. Understanding the underlying causes can make all the difference in choosing the most effective path forward.
*Note: Names and details have been changed to protect confidentiality
Resources for Parents Navigating Developmental Trauma
Supporting a child who has experienced developmental trauma requires patience, compassion, and informed strategies. Here are some valuable resources:
- The Connected Child by Karyn B. Purvis et al.: Practical advice for building trust and attachment with your adopted child.
- Parenting the Hurt Child by Gregory C. Keck and Regina M. Kupecky: This resource delves into the realities of parenting children who have experienced trauma, loss, and attachment difficulties. It combines research with real-life stories to guide parents through common challenges.
- Attachment & Trauma Network: Offers resources on attachment-based trauma and developmental trauma, with a focus on helping children and families. They also provide materials for educators and clinicians.
-

Exploring the complexity of people and their stories, finding and celebrating redemption, strength, and courage in the wake of suffering, and seeking purpose and meaning in daily life—these are the pursuits I share with my clients. Every day, I’m in awe of the impossible things they accomplish. Truly, how lucky am I? Outside of my practice, I soak up life with my husband, three kids, a house full of animals, and more chickens than I ever expected.
View all posts
 (281) 305-9387
(281) 305-9387